If you’ve been diagnosed with a peptic ulcer, you’re not alone—and you’re not powerless. At the Gastroenterology Medical Clinic in Folsom, CA, we often see patients who are surprised to learn how much their diet affects ulcer symptoms. The right foods can help you heal, while the wrong ones can aggravate the pain. This guide outlines the best and worst foods to help you manage peptic ulcers and protect your digestive health.
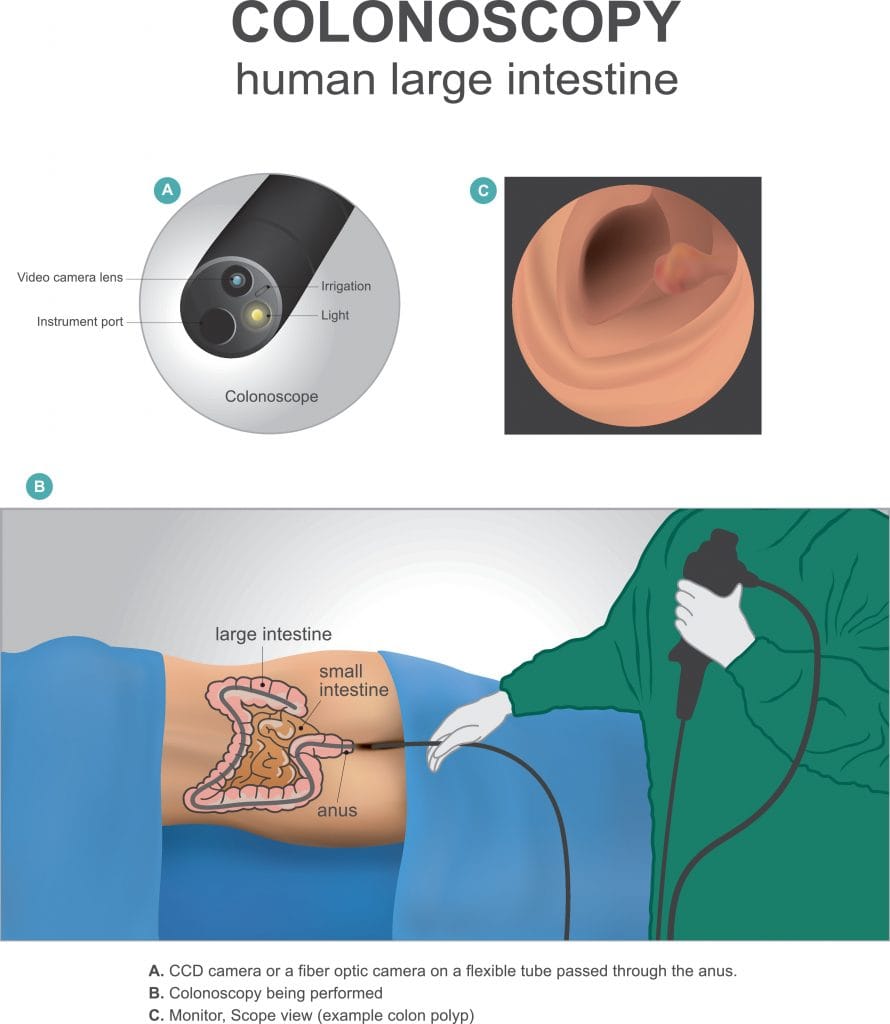
What Is a Peptic Ulcer?
A peptic ulcer is an open sore that forms in the lining of your stomach or the first part of your small intestine (duodenum). The most common causes are an infection with Helicobacter pylori (H. pylori) or regular use of NSAIDs such as aspirin or ibuprofen.
Common symptoms include:
- Burning stomach pain
- Nausea or vomiting
- Feeling full quickly
- Unexpected weight loss
If you’re experiencing any of these symptoms, we recommend scheduling an appointment with our team at Gastroenterology Medical Clinic – Folsom, CA for a full evaluation.
Why Your Diet Matters
Your diet doesn’t directly cause or cure ulcers, but certain foods can make symptoms worse or better. Acidic and spicy foods may irritate the stomach, while others help soothe the lining and reduce acid production.
Best Foods for People with Peptic Ulcers
Our Folsom-based gastroenterologists suggest the following foods to support healing and comfort:
Bananas & Melons – Low-acid fruits that help coat and protect the stomach.
Oatmeal & Whole Grains – High in fiber and gentle on digestion.
Leafy Greens & Cabbage – Full of antioxidants and natural anti-ulcer compounds.
Lean Meats & Plant-Based Proteins – Easy-to-digest proteins like chicken and tofu.
Yogurt & Fermented Foods – Promote gut balance with beneficial bacteria.
Manuka Honey – Natural antibacterial that may help reduce H. pylori.
Herbal Teas – Chamomile or licorice root teas offer soothing benefits (check with your doctor first).
Foods to Avoid with Peptic Ulcers
Avoid or limit these common ulcer aggravators:
Spicy Foods – Can increase stomach irritation.
Citrus Fruits & Tomato Products – Acidic and potentially painful.
Caffeine – Found in coffee, tea, and sodas—stimulates acid production.
Alcohol – Damages the protective lining of the stomach.
Fried and Fatty Foods – Difficult to digest and may worsen symptoms.
Chocolate – Relaxes the lower esophageal sphincter and increases reflux.
Carbonated Drinks – Cause bloating and discomfort.
Sample Ulcer-Friendly Meal Plan
Here’s a meal plan approved by our Folsom clinic:
Breakfast: Oatmeal with banana and a drizzle of Manuka honey
Lunch: Grilled chicken, steamed broccoli, and brown rice
Snack: Plain yogurt with apple slices
Dinner: Baked salmon, mashed sweet potato, sautéed spinach
Drinks: Water or chamomile tea
Helpful Tips from Gastroenterology Medical Clinic – Folsom, CA
Eat smaller meals more often.
Avoid eating late at night or lying down after meals.
Keep a food journal to identify trigger foods.
Discuss any supplements or herbal remedies with your GI provider.
When to Contact a Gastroenterologist
See a specialist at our Gastroenterology Medical Clinic in Folsom if you experience:
Black or tarry stools
Vomiting blood
Unexplained weight loss
Severe or persistent pain
These symptoms could indicate a more serious condition that needs immediate care.
Conclusion
Managing a peptic ulcer starts with smart food choices and professional care. At the Gastroenterology Medical Clinic – Folsom, CA, we help patients create personalized treatment plans that include medical therapy, lifestyle guidance, and diet education. With the right plan, you can heal faster and feel better every day.